Medical News Today Article: How can diabetes cause joint pain? Symptoms and treatment (medicalnewstoday.com)

Diabetes can cause pain in the joints in various ways. It also has links with two types of arthritis.
Over time, uncontrolled diabetes can affect the muscles and skeleton, leading to joint pain, nerve damage, and other symptoms.
Also, according to the Arthritis Foundation, almost half of all adults with diabetes also have arthritis.
Keep reading for more information about the links between diabetes, arthritis, and joint pain. We also describe telltale symptoms and the range of treatments.
How does diabetes cause joint pain?
Diabetes is a chronic condition that doctors characterize as problems with insulin and blood sugar, also known as blood glucose. Insulin is a hormone that delivers blood glucose into the body’s cells.
If a person has high blood glucose levels too often and they do not receive treatment, it can lead to a range of health conditions.
Type 1 diabetesTrusted Source is an autoimmune condition that occurs when the pancreas does not produce insulin. In contrast, type 2 diabetesTrusted Source is an acquired condition. It causes the body to produce less insulin, and the hormone does not function effectively.
There are a few different ways that diabetes can cause joint pain.
Musculoskeletal problems
Over time, if a person does not receive effective treatment, diabetes can lead to the breakdown of the musculoskeletal system. This can involve joint damage and a limited range of joint movement.
Diabetes can also cause changes in nerves and small blood vessels. As a result, hand abnormalities are very common among people with the condition.
Certain joints conditions tend to develop in individuals with type 1 or type 2 diabetes. The joint problems often correlate with the duration and control of diabetes.
These conditions include:
- carpal tunnel syndrome
- Dupuytren’s contracture, or drawing up of the palms
- trigger finger
Some people with diabetes develop thickness of the skin on the fingers along with decreased joint mobility.
They may also experience shoulder pain due to frozen shoulder or rotator cuff tendinitis.
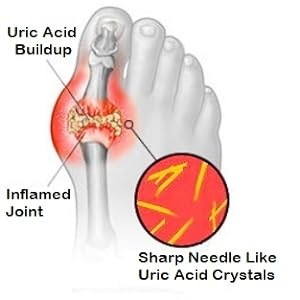
When there is damage to the joints, the cushioning no longer works as effectively. As a result, the bones can rub together, causing inflammation, stiffness, and pain. A person may also experience limited joint mobility.
Charcot’s joint
Charcot’s joint, also called neuropathic arthropathy, results from nerve damage due to diabetes. The medical term for diabetes-related nerve damage is diabetic neuropathy.
Diabetic neuropathy can cause numbness in the extremities, such as the feet and ankles. Over time, a person may feel little or no sensation in these areas. It can be easier to twist or break a foot, for example, without realizing the extent of the damage.
Small breaks and sprains can put pressure on the joints of the foot. A reduction in blood supply and mechanical factors contribute to joint damage and physical deformities over time.
In some cases, a person may be able to help prevent this damage.
The following are some warning signs of Charcot’s joint:
- redness or swelling
- numbness
- pain in the joints
- areas that feel hot to the touch
- changes in the appearance of the feet
If Charcot’s joint, or neuropathic arthropathy, is causing pain, avoid using the affected foot until it heals.
If the feet are numb, consider using additional support, such as orthotics. Doctors usually treat Charcot’s joint with a cast.
Rheumatoid arthritis and type 1 diabetes
Both rheumatoid arthritis (RA) and type 1 diabetes are autoimmune disorders, meaning they both cause the immune system to attack an otherwise healthy part of the body.
In a person with RA, the immune system attacks tissues in the joints, causing swelling, pain, and deformities. And in an individual with type 1 diabetes, the immune system attacks the pancreas, stopping the production of insulin.
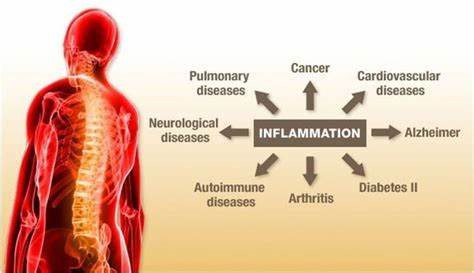
Both RA and type 1 diabetes involve inflammation, and certain clinical signs of inflammation — including C-reactive protein and interleukin-6 levels — are consistently high in people with either condition.
Having one autoimmune condition can increase the risk of developing a second. This helps explain why type 1 diabetes and RA can coexist.
Osteoarthritis and type 2 diabetes
Unlike type 1 diabetes, type 2 has strong links to excess body weight. Being overweight or having obesity also increases a person’s risk of developing osteoarthritis (OA), as the weight puts extra stress on the joints, particularly in the lower body.
A person can reduce their risk of developing type 2 diabetes and OA by maintaining a moderate weight through a nutritious diet and regular exercise.
If a person has either condition or both, reaching and maintaining a moderate weight can improve symptoms. According to the Arthritis Foundation, studies show that losing 1 pound (lb) of weight in people with overweight or obesity can result in losing up to 4 lb of pressure on the knees. Alternatively, losing 10 lb can relieve 40 lb of pressure from the knees.
Additionally, in a person with type 2 diabetes, losing 5–10% of their total body weight can reduce their blood sugar levels significantly. As a result, they may need to take less medication for the condition.
Treatment and management
Taking over-the-counter (OTC) anti-inflammatory medications, such as ibuprofen, can often reduce pain and swelling in the joints. Individuals can speak with a doctor about how much ibuprofen is too much in the short and long term.
If joint pain and other symptoms persist, people can discuss treatment options with a doctor. Some individuals may benefit from braces, orthotics, adjustments to their lifestyle or medication, or a combination.
Type 1 and type 2 diabetes have different causes and treatments. People with type 1 diabetes usually need to take insulin to control their blood sugar levels.
Individuals with type 2 diabetes may also require insulin. Often, they only need to take medication that improves their insulin response to blood sugar.
People with either type of diabetes can benefit from maintaining a nutritious diet and daily exercise. Reaching and maintaining a moderate weight has additional benefits for those with type 2 diabetes.
Additionally, receiving early treatment can help a person avoid long-term diabetes complications, such as joint damage and malformations.
Prediabetes and joint pain
Maintaining a moderate weight can help a person reduce their risk of prediabetes and joint pain.
Excess weight can lead to higher blood sugar levels, and the pancreas may be unable to produce enough insulin to keep up. This can cause a person to develop type 2 diabetes.
Carrying excess weight also puts stress on the joints, particularly in the lower body.
To reduce the risk of developing type 2 diabetes and limit stress on the joints, a person should maintain a moderate weight. They can often do this by exercising regularly and eating a nutritious diet of whole grains, vegetables, fruits, and lean proteins.
Summary
Without effective treatment, diabetes can cause joint pain.
The pain can result from the effects of diabetes on the musculoskeletal or nervous systems. Joint pain can also occur if diabetes has links to arthritis, such as RA or OA.
In some people, OTC pain relievers and anti-inflammatory medications are enough to reduce joint pain. Others may need additional treatment.
Eating a nutritious diet, getting regular exercise, and maintaining a moderate weight can help improve symptoms and prevent complications.
Gluco100®- Glucose Management
Are you pre-diabetic? Already over 100?
Two tests are comm…
Flamasil® for Inflammation & More
Flamasil™
(for General Joint Pain, Arthritis, Gout, Body Inflammation, and Cellular Health)
— Are you aware that uncontrolled inflammation can lead to Heart Disease, Diabetes, and even Cancer?
— You must remove chronic inflammation from your life b…



Leave a Reply